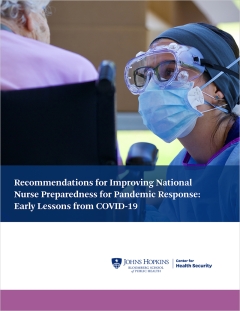
Nursing is the largest health profession, with nearly 4 million providers practicing across acute, primary, and public health care settings. In response to the pandemic, nursing schools halted on-site course delivery and redesigned programs to attenuate risks to students and faculty. Key challenges faced by schools included financial cutbacks, rapid increases in online learning technology, maintaining student academic progression, disruption to clinical learning opportunities, and meeting accreditation standards, while addressing the stress and loss experienced by faculty, staff, and students. Despite challenges, nursing organizations provided guidance for decision making, new learning resources, and faculty development opportunities. Schools of nursing leveraged their resources to redesign nursing curricula, strengthen partnerships for student clinical experiences, and address needs of the community.
Nursing education will look different from its prepandemic profile in the future. Lessons learned during the pandemic point to gaps in nursing education, particularly related to disaster and public health preparedness, health equity, and technology. The American Association of Colleges of Nursing’s new Essentials—standards for professional nursing education—were finalized during the pandemic and reflect these lessons. The need for nurse scientists to conduct emergency response research was made evident. The importance of strong academic–practice partnerships was highlighted for rapid communication, flexibility, and responses to dynamic environments. For the future, nursing education and practice must collaborate to ensure that students and practicing nurses are prepared to address emergencies and pandemics, as well as the needs of vulnerable populations.